Nuances of Observational Studies of Time-to-Antibiotics and Sepsis Mortality
I’m happy to announce a research article I published in Clinical Infectious Diseases with my mentors Mike Klompas and Chanu Rhee, entitled “Risk of Misleading Conclusions in Observational Studies of Time-to-Antibiotics and Mortality in Suspected Sepsis.” The full text is freely available using this link.
We were motivated to perform this study after we reviewed the state of evidence used to support clinical guidelines on timing of antibiotics for sepsis. The typical maxim given on rounds is that the risk of death increases by 8% per hour of delay in treatment, and this has been sloganized into phrases like It’s About TIME.
Essentially all evidence for this derives from observational cohorts. A close reading of these studies shows four potential areas of concern, including:
- limited adjustment for potential confounders,
- inclusion of outlier patients with very long delays until antibiotics,
- failure to differentiate between sepsis with and without shock, and
- use of linear models that assume that each additional hour until antibiotics has an equal effect.
We created our own cohort that compares favorably to prior studies (largest N, five hospitals, detailed patient-level clinical data) and tested each of these analytical concerns in turn. (In essence, this was a series of four sensitivity analyses.) We used the same basic method as the most prominent studies in this field (multivariable logistic regression), varied the assumption corresponding with each analytical concern, and checked if the results changed. For all four, they did.
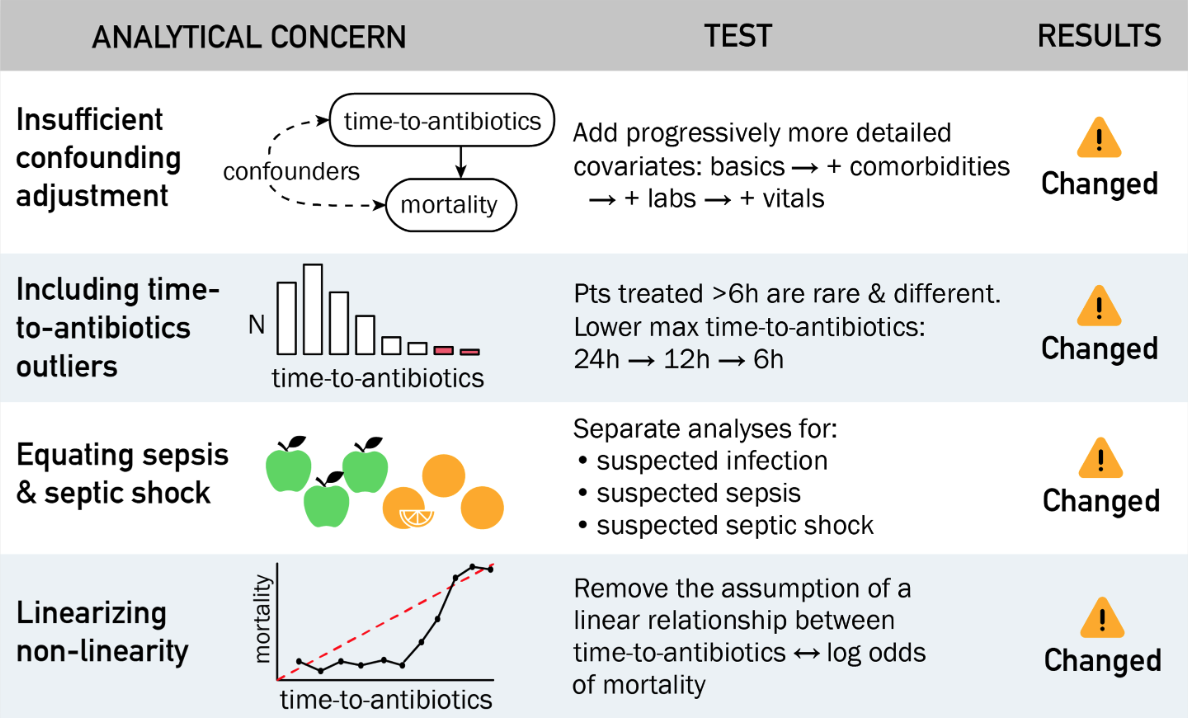
We conclude that this type of study is highly sensitive to analytic choices regarding confounding, outliers, inclusion criteria, and non-linearity, and it’s likely that most of the prior studies were afflicted by at least one of these problems.1 If we keep only the most conservative assumptions (shorten the study time to 6h and adjust for all possible confounders) we are able to find a significant hourly relationship in patients with shock, but not in the cohorts without shock.
Many thanks to the entire Sepsis Time Zero team, TIDE, and the Harvard ID T32 for supporting this work, as well as the American Thoracic Society for inviting me to speak about it at the 2023 meeting.
-
The many, many pitfalls of time-to-intervention studies are summarized in this evergreen EMCrit post by Josh Farkas. ↩
Discuss this post on HN.